Mission Statement
The Environmental Public Health Program supports Northwest Tribes in creating wellness for the seventh generation.
Purpose Statement
The Environmental Public Health Program supports Northwest Tribes by providing comprehensive environmental public health services grounded in Indigenous knowledge and western science.
HEALTH ALERT NOTICE
Dear colleagues, This Health Alert Notice requests providers be alert for and report cases of Paralytic Shellfish Poisoning. OHA has received reports of multiple cases of Paralytic Shellfish Poisoning since May 25,2024. Cases have reported consumption of shellfish from North Oregon Coast beaches.
Expand below to read further:
Health Alert Notice: Paralytic Shellfish Poisoning
Dear colleagues,
This Health Alert Notice requests providers be alert for and report cases of Paralytic Shellfish Poisoning.
OHA has received reports of multiple cases of Paralytic Shellfish Poisoning since May 25,2024. Cases have reported consumption of shellfish from North Oregon Coast beaches.
Paralytic shellfish poisoning (PSP) is the most common and most severe form of shellfish poisoning.
- PSP is caused by ingestion of bivalve shellfish that have accumulated saxitoxin as well as several other neurotoxins. These neurotoxins are produced by cyanobacteria and dinoflagellates and accumulate in filter-feeding shellfish like mussels, clams, oysters, and scallops.
- PSP occurs worldwide but is most common in temperate waters off the Atlantic and Pacific coasts of North America.
- Signs of illness usually appear 30–60 minutes after a person eats toxic shellfish and include numbness and tingling of the face, lips, tongue, arms and legs. Patients also might have diarrhea and vomiting, headache, and nausea.
- Severe cases are associated with ingestion of large doses of toxin and clinical features such as poor muscle control, clumsiness or slurred speech, difficulty swallowing, loose or floppy limbs, mental status changes, and respiratory failure.
- Paralytic shellfish poisoning can be deadly, especially for children. Appropriate medical care can lessen the risk of death.
Prevention
- Shellfish poisoning can be prevented by avoiding potentially contaminated shellfish, which is particularly important in areas during or shortly after algal blooms, locally referred to as “red tides” or “brown tides.”
- Avoid harvest and consumption of seafood from beaches with biotoxin closures.
- Consuming shellfish also carries a very high risk for infection from various viral (e.g., hepatitis A virus, norovirus) and bacterial (e.g., Salmonella, Shigella, Vibrio parahaemolyticus, and vulnificus) pathogens. Ideally, travelers to developing countries should consider avoiding eating shellfish.
- It should be noted that:
-
- Marine shellfish toxins cannot be destroyed by cooking or freezing.
- Shellfish containing paralytic shellfish toxin may not look, smell, or taste any different than uncontaminated shellfish.
- Crabs may feed on shellfish and, therefore, might also have the toxin.
- Pets and service animals should also not eat potentially toxic shellfish.
Treatment
There is no antidote or specific treatment. Treatment is symptomatic and supportive.
- Severe cases of paralytic shellfish poisoning might require mechanical ventilation.
- If the ingestion was recent (within 2 hours), and it is safe to do so, a single dose of activated charcoal (50g in adults, 1 mg/kg in children) is reasonable.
Key contacts:
- Call the Shellfish Biotoxin Hotline before sport harvesting Toll free: 1-800-448-2474.
- Please contact the Oregon Poison Center (1-800-222-1222) if you encounter a suspected case.
- Please contact your local public health agency to report any suspected cases. For a directory of contacts visit: https://www.oregon.gov/oha/ph/providerpartnerresources/localhealthdepartmentresources/pages/lhd.aspx
- Or, contact the Oregon Health Authority’s 24/7 disease reporting line at 971-673-1111.
For additional information:
- Centers for Disease Control and Prevention: https://wwwnc.cdc.gov/travel/yellowbook/2024/environmental-hazards-risks/food-poisoning-from-marine-toxins
- Oregon Department of Agriculture Recreational Shellfish Biotoxin Closure: https://www.oregon.gov/ODA/programs/FoodSafety/Shellfish/Pages/ShellfishClosures.aspx
- Oregon Department of Fish and Wildlife Shellfish and Biotoxins: https://myodfw.com/articles/shellfish-and-biotoxins#:~:text=Paralytic%20Shellfish%20Poisoning%20(PSP)%3A&text=People%20who%20eat%20shellfish%20that,occur%20within%20hours%20of%20consumption.
- Oregon Health Authority Fish and Shellfish Consumption Resources: https://www.oregon.gov/oha/ph/healthyenvironments/recreation/fishconsumption/pages/seafood-shellfish.aspx
This HAN was sent to ORCD1 and PIO rules, which includes local and tribal health officers, administrators, PHEP Coordinators, public health information officers, other public health emergency response partners, and some OHA staff.
_______________________________________________________________
Unless otherwise noted, feel free to share this HAN notification with:
– Others within your organization.
– Professionals within your health, preparedness, and response affiliations.
Oregon 24/7 disease reporting: 971-673-1111
OUR TEAM







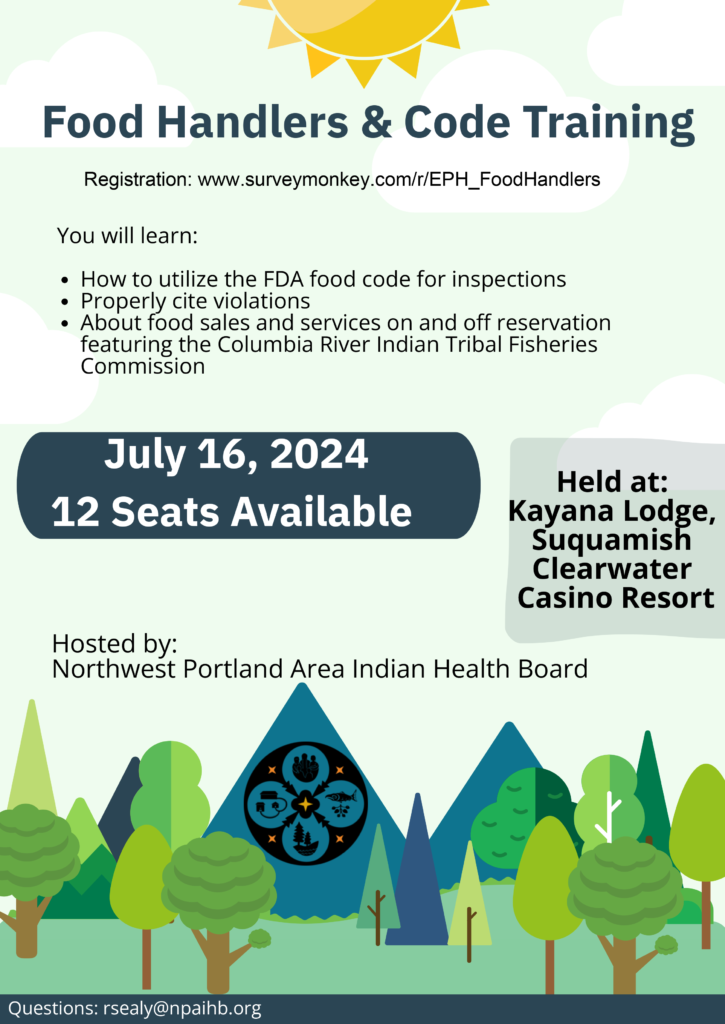
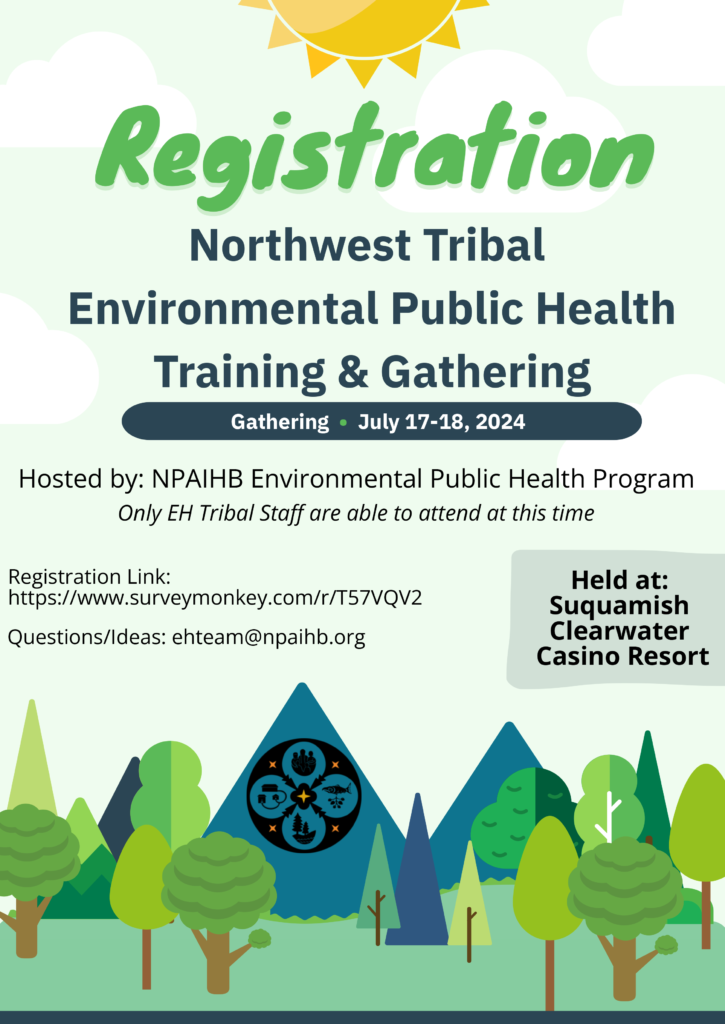
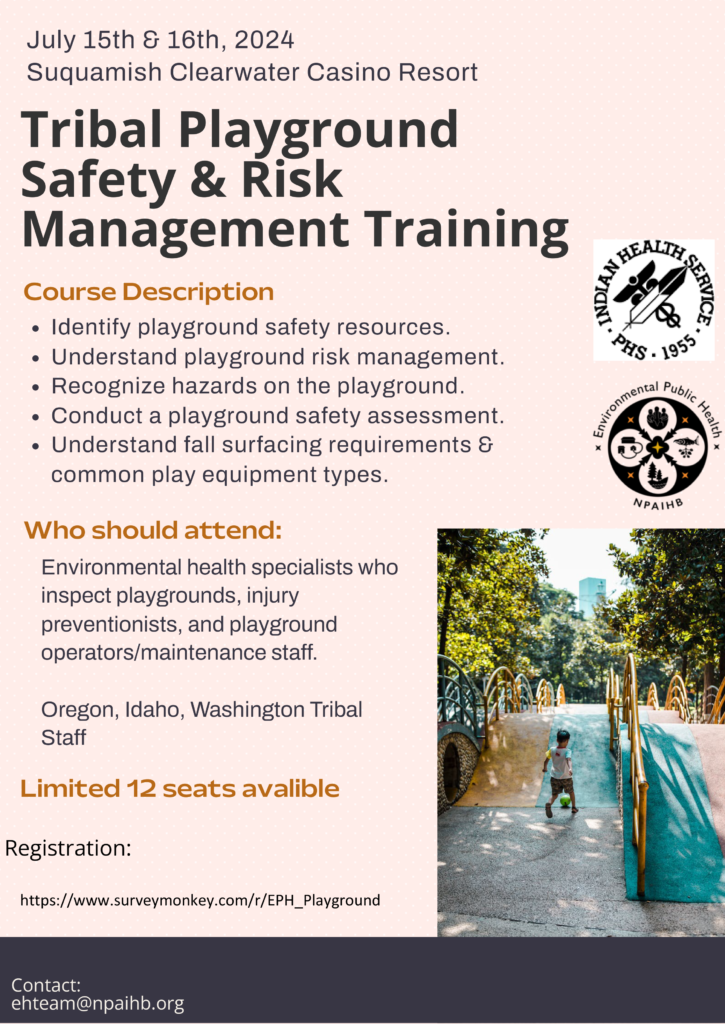
UPCOMING EVENTS
SERVICES
Core
Projects
- Accreditation Association for Ambulatory Health Care Accreditation Readiness
- Homes
- Schools
- Food
- Water
- Attendees: Pacific Northwest Tribes
- 2022 Topics: Environmental Health Definition, Tribal Ecological Knowledge, Shared Indicators
- CEHA Profiles
- Community Environmental Health Improvement Plans
- Tribal Profiles and Story Maps
- CEHA Profiles
- Community Environmental Health Improvement Plans
- Tribal Profiles and Story Maps
- Qualitative Collection and Analysis
- COVID-19 After Action Reviews
- Action Planning, Tabletop Drills, Hot Wash Facilitation
- Annual Tribal Public Health Emergency Preparedness Conference
- FEMA Preparedness Training
CONTACT US
Please reach out to us via the form to the right, or email us at:
ehteam@npaihb.org